A Future Where CB1 Is Visible
The CB1 Number On Your Phone
Right now, the endocannabinoid system is mostly guesswork in the clinic.
People come in with pain, anxiety, insomnia, autism-related challenges. They describe what they feel. Clinicians adjust oils, flower, edibles, ratios. Some patients improve, some don’t, and many just hover in a gray zone of “maybe this helps a bit.”
Tolerance builds slowly. Side effects accumulate slowly. And through all of it, one crucial question never gets a real answer:
”How much CB1 receptor capacity does this person actually have, right now?”
Is this someone whose CB1 system is fresh and responsive? Someone who is already downregulated after years of daily use? Someone in the middle of recovering after a long break?
We do not see it. We just feel around it.
Now picture something different.
How CB1 Availability Changes Medical Cannabis
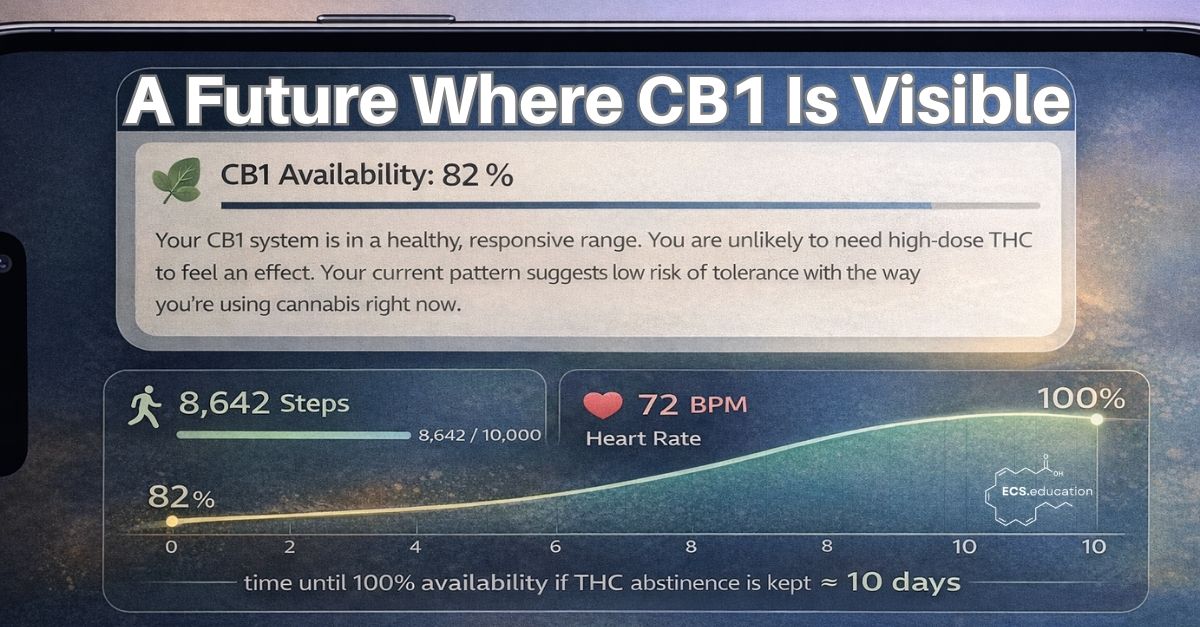
Imagine opening your phone and seeing an “ECS Health” panel next to your step count and heart rate. At the top, there is a simple line:
CB1 Availability: 82 %
Underneath, a few sentences in plain language:
“Your CB1 system is in a healthy, responsive range. You are unlikely to need high-dose THC to feel an effect. Your current pattern suggests low risk of tolerance with the way you’re using cannabis right now.”
That number is not a mood score. It is not a questionnaire. It is the end result of a non-invasive biomarker system that has been quietly listening to your physiology over days and weeks, then translating it into one piece of information you and your clinician can both understand: how much CB1 “bandwidth” you have.
All the complexity is under the hood. On the surface, there is just a clear, stable signal that answers the question we currently treat as unanswerable.
First prescriptions stop being blind guesses
Think about what that changes in a very ordinary clinic visit.
A patient with chronic neuropathic pain walks in. Today, the default is a careful version of trial and error: start low, go slow, adjust, hope.
In this other world, the first thing the clinician looks at is the patient’s ECS Health panel:
- CB1 Availability: 38 %
- ECS Stability: low, jumping around over the past month
- Tolerance: clearly rising
The conversation changes. High-dose THC isn’t just “maybe too much,” it is flagged as something that will probably push an already strained CB1 system further down. The digital assistant suggests CB1-sparing options: more balanced THC:CBD, non-THC ECS modulators, non-cannabinoid co-therapies. Patient and clinician build a plan that treats CB1 as a limited resource to be protected, not an invisible receptor that can be hammered harder whenever symptoms flare.
Symptom relief still matters. But now it is balanced against maintaining CB1 capacity over years, not just days.
Tolerance and recovery are no longer guesswork
The same applies to tolerance and “tolerance breaks.”
Today, most people realize they are tolerant when the usual dose does nothing, and they decide to stop for a while when they are frustrated or worried. They hope a break helped. Nobody really knows by how much.
In a CB1-visible world, a heavy long-term user might open the app and see:
CB1 Availability: 22 %
“You are in a CB1-depleted state. If you keep using at this level, you are unlikely to regain sensitivity. If you reduce or pause, we estimate roughly 6–8 weeks to reach 60 %.”
If they do choose to pause, they can actually watch CB1 climb:
- Week 2: 35 %
- Week 4: 51 %
- Week 6: 64 %
At some predefined point, their clinician gets a notification: CB1 capacity is back in a safer zone if re-starting low-dose THC still makes sense clinically.
Instead of “I think my system reset,” there is a curve. People can still listen to their bodies—but now they have an extra sense.
Precision ECS medicine in neurodevelopment and psychiatry
This doesn’t only apply to adults with pain or insomnia.
Imagine a teenager on the autism spectrum, struggling with sleep, sensory overload, and daytime behavior. Right now, families and clinicians might try CBD, low-dose THC, or other ECS-focused strategies mostly in the dark. If something helps, they keep going. If it backfires, they stop. The underlying ECS remains invisible.
In the world being described, that teenager has a longitudinal trace of CB1 availability, side by side with sleep quality, daytime behavior, sensory thresholds, mood. Over time, patterns start to emerge.
Some kids show low CB1 availability with high instability. They do best when the initial focus is on stabilizing and gently restoring CB1 capacity first, before cannabinoids are pushed. Others show normal CB1 availability but clear downstream dysregulation. They may benefit more from ECS-modulating adjuncts and targeted co-therapies than from directly driving CB1.
Clinical trials shift accordingly. Instead of “ASD with insomnia” as an inclusion criterion, you might see “ASD with CB1 availability below 40 % and unstable ECS dynamics.” Trial outcomes are not just changes on behavior scales; they also track whether CB1 availability is moving toward a healthier, more stable range.
In other words, neurodevelopment and psychiatry start to use ECS biology as an axis, not just symptoms.
Safer, smarter regulation and product design
Regulation and product design also look very different in this kind of world.
Right now, debates about impairment and safety often revolve around blood THC levels. But anyone who has worked closely with cannabis knows how incomplete that is. Two people can have the same THC concentration in their blood and wildly different levels of cognitive and motor impairment. One is fragile and easily overwhelmed. One is highly tolerant and barely fazed.
The missing piece in that comparison is CB1.
Once CB1 availability enters the picture—even in anonymized, aggregated form—real patterns appear:
- Some product types and dosing habits reliably push CB1 down and keep it there.
- Other approaches, especially when combined with supportive protocols, allow CB1 to stay stable or even recover over time.
- The link between a certain blood THC value and actual impairment looks very different at 80 % CB1 availability than it does at 25 %.
Regulators now have something more meaningful to work with than a single THC cutoff. Instead of rigid “per se” limits that assume everyone at a given THC level is equally impaired, rules can start to acknowledge that individual CB1 state is a major piece of the puzzle. Over time, frameworks can evolve where both THC concentration and CB1 availability inform decisions about risk, fitness to drive, or occupational safety.
Product developers also stop designing in the dark. They can build explicitly CB1-friendly formulations and usage patterns that deliver benefit without quietly chewing through receptor capacity. Public health guidance can move away from vague slogans and toward specific, biomarker-based advice:
“If your CB1 availability is below this range, avoid that pattern. If your CB1 availability is above this range, these options are generally safe—provided objective impairment measures remain within limits.”
Instead of arguing whether cannabis is “good” or “bad,” the conversation can finally center on responsible, data-guided stewardship of a system that clearly matters.
A Day in the Life of ECS Medicine
Day to day, this doesn’t look like sci-fi. It looks like ordinary care with one extra sense.
A patient opts in to ECS monitoring through the same ecosystem that already handles their other health data. A non-invasive biomarker system builds, quietly, a personal model of CB1 and ECS stability over time. When it’s time to start, adjust, or stop cannabinoids, patient and clinician look at three simple things together:
- Where is CB1 right now?
- Where has it been trending?
- How will each option likely affect that trajectory?
From there, treatment modes become more intentional:
- A CB1 preservation mode for chronic conditions that need long-term stability.
- A CB1 restoration mode for people coming back from heavy use or adverse experiences.
- A CB1 augmentation mode when short-term, more forceful interventions are justified, but carefully monitored.
The phone that used to just buzz with “time to take your dose” becomes a window into how the ECS itself is changing—and a guardrail against slowly grinding CB1 into the ground without noticing.
From Black Box to CB1 Biomarker
Right now, ECS medicine is powerful but opaque. CB1 is central to why medical cannabis helps some people so much, why it stops working for others, and why a subset run into real trouble. Yet CB1 itself never enters the chart as a number.
In the scenario above, CB1 availability becomes just that: a number you can see. Once that happens, a lot of things that currently feel fuzzy suddenly become:
- Measurable rather than assumed,
- Personal rather than generic,
- Preventive rather than purely reactive,
- And genuinely shared, as patients and clinicians look at the same CB1 curve and make decisions together.
It also becomes more fair. Discussions about safety, impairment, and access can finally include the individual CB1 factor that has always been there, but has never been visible.
Closing the Loop: From Vision to CB1 Availability Proof of Concept
This is written as a vision of the future, but it is far from entirely theoretical.
A proof-of-concept technology already exists that uses non-invasive physiological signals to separate CB1 states in real people. Early results show a clear separation between heavy long-term use and cannabis-naive controls. More detailed data is available under NDA.
The next step is to turn these early results into a robust platform: a CB1 biomarker system that can support exactly the kind of ECS-guided medicine described here, and eventually change how medical cannabis is prescribed, monitored, and regulated.
If you are building in this space—as a clinician, researcher, operator, or investor—and you want to help move ECS medicine from black box to biomarker, the door is open. The goal is simple to state and ambitious to execute:
Make CB1 visible, and use that visibility to make cannabis care safer, smarter, and more humane.
Stefan Broselid, Ph.D.

Comment
Comments are closed.